Tom Robinson (Chatham 97)
I have no idea how I have survived nearly two decades of brutal suffering at the hands of severe type 1 bipolar disorder.
I spent months, even years sometimes, ‘dying to stay alive’, in bed, desperately trying to resist my suicidal thoughts and intentions with the curtains firmly closed; achieving nothing, going nowhere and seeing no one.
But against all odds, I have not only survived this horrific ordeal, but I’ve stabilised, reached remission, recovered and reclaimed my life; quite how I’ve managed to do this is so astonishing that it has left me with an unrelenting determination to share my story as widely as possible, in an attempt to help and educate others.
There were no obvious signs that I would fall victim to the brutality of a severe mental illness. I had pretty much breezed through my school years at Stowe where I achieved good grades, participated keenly in sports and activities and took advantage of the multitude of opportunities that were available to me.
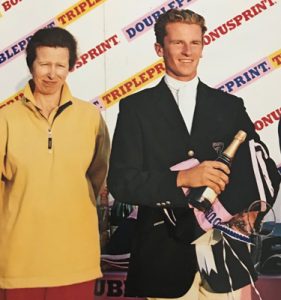
But there was one dream I was intent on following above all else because my grand passion lay in equestrianism – and I had a dream of being an Olympic three-day event rider.
Fortunately, my Headmaster, Jeremy Nichols, and Housemaster, Tony Meredith, were supportive of my ambitions but since there were no equestrian facilities at Stowe at the time, I would sneak out of school to ride at almost every opportunity. I’m not sure quite how seriously my Masters and Housemates took me, before I won the Junior National Championships in the first year of my A-levels, after though, they seemed to take a much keener interest!
Later that same summer, I was selected to represent Great Britain in the Junior European championships where we won a team gold medal; further fuelling my ambition to succeed at the highest level.

in August 2002
This taste of success made me hungry for more, so with the support of my parents I started competing professionally after finishing school.
Successes at the bigger three-day events followed, with placings at Bramham, Chatsworth and Blenheim as well as taking a national title at Gatcombe and completing my first Badminton. But while achieving all of this, I was battling my own mind, with my mood mimicking the ups and downs that so often go with the sport of eventing.
One autumn afternoon everything came to a head. I had been suffering from exhaustion for months, yet battling on regardless, determined to keep going and competing, mostly because I was terrified of admitting a problem and ashamed that I was feeling so down. I continued, largely by beating myself over the back mentally with a stick, and faking being alright, until one day in September of that year I just couldn’t take it anymore and I completely broke down. I went to a doctor who diagnosed me with depression and prescribed me with antidepressants.
There began my psychiatric nightmare which would last twenty years and take every ounce of perseverance and resilience to survive. Competing became impossible and eventually I had to give up everything and go to bed in my parent’s house, completely dependent on them for everything and sleeping constantly to avoid the mental pain.
Throughout the twenty-years of this nightmare ordeal, I have been medicated, time and again, with a myriad of different treatments and therapies, yet not one of them has worked in even the slightest way. In fact, all that the traditional psychiatric drugs did, was to make my condition so much worse!
This has meant that I have been fighting so much more than just the vicious onslaught of bipolar episodes, because I’ve had the side effects of the drugs, the withdrawal problems when they failed me and the disappointments and failures to contend with too – a hideous situation and a potentially very dangerous one too.
The initially prescribed antidepressants such as citalopram, fluoxetine and sertraline, induced such panic and fear that I was left constantly on a knife-edge, sweating, trembling and having to endure crippling bouts of increased agitation, mixed with heightened swirls of terrifying anxiety.
I now recognise that I was experiencing a ‘mixed affective state’ as a direct result of the antidepressants, where I was suffering from depressed and manic features at the same time!
It was at this juncture where I believe my bipolar disorder (as opposed to unipolar depression) first originated, yet all of these obvious symptoms went undiagnosed because the extent of the care I received was so cursory, inadequate and frankly – grossly negligent and substandard.
In those early episodes I would like awake all-night-long with crippling insomnia, paralysed with fear and dreading the first bird song which, for me, would signal the start of another day of ‘faking it’ as a competent and successful international event rider.
Mood stabilisers such as lithium and sodium valproate were introduced which again did nothing to alleviate my depression yet added only more complications and side effects. At one point I developed a particularly distressing and itchy bout of hives which broke out in their thousands all over my back. I remember thinking:
I already want to kill myself and now I’m sweaty and spotty – I really don’t think I can take any more than this – please God – just let me die!
By this point I’d pretty much decided to either take my own life or find an alternative route out of the hell, so for a while I tried to manage my illness without medication, but when my depression returned with a vengeance in 2017, I found myself desperate again and I made the fateful decision to return to the NHS medical profession for help and guidance.
By this point I had been forced to relinquish my Olympic dream of representing Great Britain in the sport of three-day eventing and had decided that studying psychology at university might bring a change of focus and perhaps some answers too, but unfortunately this ambition would only be ripped away from me too.
The combination of subthreshold depression, combined with exam pressures and the general verbosity of the subject itself, dragged me to the point of desperation once more, so when a friend alerted me to the fact that they were using ketamine to treat resistant cases in nearby Oxford, I immediately applied for an assessment.
This would prove to be a near fatal decision because the treatment that was being hailed as a ‘miracle cure’, backfired so spectacularly that it very nearly cost me my life.
Having sobbed my way through the entire assessment, I was duly accepted for treatment with ketamine, which was to be administered intravenously, once a week, over the course of the following three weeks.
The first infusion took me on a frightening psychedelic trip but did absolutely nothing to alleviate my depression. By the time I went back for the second treatment I was in mental agony with almost catatonic depression. I sat on the waiting room floor crying in pain and desperation.
The psychiatrist firstly, told me off for openly expressing my suicidal thoughts and then threatened to ban me from the clinic after I collapsed on the floor in crisis. The extent of the support was abysmal and it horrifies me that some of the most vulnerable people in society are being subjected to such an appalling lack of basic care, empathy and common courtesy and consideration.
The second infusion was equally as hideous as the first and I went home to bed and collapsed in pain and suffering as usual.
Over the next four days my sleep pattern went from 17 hours a day with ‘simple’ depression, to the absolute opposite end of the spectrum where I experienced complete mental disruption, getting absolutely no rest at all, let alone anything resembling relaxation and sleep.
I was now terrified that mania was on its way to me because I knew the pattern from previous episodes, but there was no follow-up between appointments, so I wasn’t able to express my concern with a professional. Repeated attempts proved fruitless and the response to my urgent email was an auto ‘out of office’ reply which left me in panic and fear with an ever-growing feeling of desperation and anxiety.
Eventually, after much persistence, I did get hold of a healthcare assistant whose advice was to take a herbal sleeping pill!
For what happened next, I hold the clinic entirely responsible.
I was now well on my way to mania yet the chance to help me was well and truly gone. I was spiralling out of control and unable to form a balanced perspective on my own condition.
By the time of the next appointment, I was in a full-blown manic episode, literally flying around at a million miles an hour, believing that I was some kind of biblical prophet or disciple, blessing people with holy water and rambling and pontificating about philosophical and psychological dilemmas like Cartesian dualism and the mind-brain problem.
Ketamine had propelled me from the depths of despair to unbridled euphoria in the space of two weeks, but I was now in an even worse situation than before because I was sectioned and incarcerated on a chaotic psychiatric ward for the next three months.
During this traumatic admission, I was overpowered and bulldozed in a corridor twice and forcibly injected with sedatives and antipsychotics – all of this could have been avoided if only I’d had access to support, emergency contact, follow-up and earlier medical intervention. It terrifies me that this could potentially happen to someone else because I know that what I’ve experienced as a result isn’t really survivable.
I was placed under the care of a completely different psychiatrist who had absolutely nothing to do with the ketamine treatment and I spent the whole summer trying to explain what had happened, yet I was consistently misunderstood and discredited, with every action being interpreted as symptomatic of mania and madness.
Support in hospital in the form of therapy or counselling was non-existent. In fact, the care was so appalling that when I realised that I would be receiving no beneficial input from the staff, I resorted to putting my earphones in, blocking out the pandemonium and talking to no one.
The only thing that kept me going in those difficult months of 2017 were the other patients. Eighteen amazing men ranging from the age of 18-65 with every kind of mental ‘disorder’ imaginable, all of whom were incredible.
Several of them made an impression on me, but there was one guy in particular whose strength and resilience stood out to me. He had attended Eton College and we spent hours laughing at the ridiculousness of the situation. We both agreed that we were able to survive ‘ward life’ because of the resilience and ‘never give up’ attitude that was instilled in us through public school.
When I was finally discharged my mood dropped from ‘stable’ (in reality; emotionally damaged and traumatised) to suicidal, in a matter of about a month and I spent the next 18 months in a catatonic depression, barely leaving my room, let alone the house, constantly having to resist the suicidal thoughts that dominated my every waking moment.
During 2018, I went back to the ketamine doctor and (believing that I had no other option) underwent nearly a whole year of treatment with oral ketamine, which was not only revolting but completely ineffective.
Even at higher doses where I would experience a horrific ‘k hole’ (where I was completely detached from every human concept), my depression did not lift in even the slightest way.
All the other patients that were undergoing treatment alongside me reported no benefit from ketamine either and we would return week in, week out totally demoralised and in suicidal crisis, despite our continuous trips for more downing of the revolting horse tranquilizer at the hospital.
I eventually gave up with ketamine completely and, although I was still desperate for medical intervention, having had my condition so much worsened I vowed never to go back to the NHS for mental healthcare ever again.
By this point, I had virtually given up all hope of survival, when in early 2019, a friend contacted me and begged me to make an appointment to see her private doctor, at the very least for an assessment. So, I took a deep breath and decided that before I made the decision to permanently end things, I would give this one last try.
I first went to see Dr Andy Zamar at the London Psychiatry Centre on Harley Street at the end of March 2019. I knew that I didn’t have the strength to divulge the horrific truth of the illness, so I wrote the full horror story down before I went.
He identified almost immediately that, as a result of everything that had happened, I was now rapid cycling between ‘simple depression’ (there’s nothing simple about it), ‘mixed state’ (manic negative thoughts), ‘agitated depression’ (where I felt deep inner unrest, my heart twinging constantly) and ‘depression with flight of ideas’ (negative ruminations, constantly returning to thoughts of hanging and suicide).
Dr Zamar took me extremely seriously and went on to question me extensively about my symptoms and experiences – something no other psychiatrist had ever done in twenty years.
I walked out of the appointment feeling for the first time in two decades, educated about my condition and almost more importantly HEARD – my feelings were valid and the seriousness of my situation had been finally appreciated.
After the appointment, I said to Mum:
This man will be enough to save me because he understands.
There were no deliberations, waitlists or delays and I started a combined treatment with high dose levothyroxine and rTMS (repetitive transcranial magnetic stimulation) with immediate effect.
The progression to full remission was steady and took longer than usual because of the damage caused by the failed treatments, but within the space of a few months, things started to become easier.

Eight months of treatment with rTMS and a titration up to 800mcg of levothyroxine has restored my brain to its original equilibrium, which, after the obliteration of virtually every neurotransmitter and chemical is, quite frankly, a miraculous achievement!
The journey to remission has taken much persistence, patience, resilience and determination, combined with a huge amount of introspection and self-analysis. I’ve had to make a conscious effort to work through the trauma, reconcile with the past and fully move on with my life. This has not been easy at all and has been made even more complicated by the forced antipsychotics which I have only just managed to withdraw from – something I write extensively about on my blog.
I am now very proud and also extremely relieved to say that I am finally back to the authentic version of myself; I don’t doubt my brain, I don’t have to fight to get out of bed in the morning and I’m relaxed and happy with life.
I believe the route to full mental wellness is a combination of many, many things which this novel treatment has given me the foundation to work from. I now enjoy exercising, looking after myself through attending to my diet and have been more than happy to cut out all of the unhelpful ‘crutches’ that I once depended on, such as nicotine, caffeine and alcohol.
This experience has changed me profoundly and nothing now matters except staying well and helping others to survive and recover.
Somehow, between episodes, I managed to complete an NCTJ in journalism and am now finally using my qualification, over ten years later, to write and document all that I’ve learnt on this journey back to life.
I have detailed the whole story in a combined memoir and self-help book in order to warn others of the dangers of iatrogenic harm, as well as alert them to this ground-breaking and revolutionary approach to treating bipolar disorders. I am currently seeking literary representation for this and in the meantime am sharing as much gratuitous information on my website as possible. This can be found here.
In September, I started training in NLP (neuro-linguistic programming) and I hope very much to be able to spread a huge amount of hope and understanding around bipolar, as well as many other mental illnesses and disorders.
Please don’t hesitate to get in touch should you need help, guidance, support, or if you wish to know any other details of this story.

